Η Lapin House αφιερώνει το υπέροχο σοκολατένιο αυγό της σε σχήμα αρκουδάκι στη «ΓΑΛΙΛΑΙΑ»
Με κάθε σοκολατένιο αυγό που θα αγοράζετε από τα καταστήματά της, η Lapin House θα δωρίζει μέρος της αξίας του στους ασθενείς της «ΓΑΛΙΛΑΙΑΣ».
Τι επαγγελματικές και εκπαιδευτικές ευκαιρίες υπάρχουν στη «ΓΑΛΙΛΑΙΑ» για εμένα;
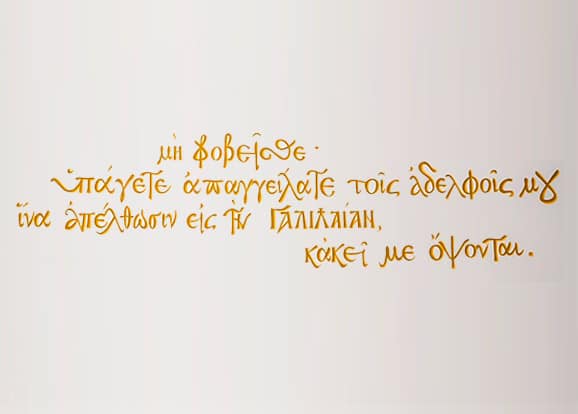
H «ΓΑΛΙΛΑΙΑ» είναι μια Πρότυπη Μονάδα Ανακουφιστικής Φροντίδας, η μοναδική στη χώρα μας που προσφέρει δωρεάν ολοκληρωμένες υπηρεσίες Ανακουφιστικής Φροντίδας σε ασθενείς με καρκίνο και ασθενείς με νόσο του κινητικού νευρώνα (ALS) μέσω εξειδικευμένης διεπιστημονικής προσέγγισης.
Η Ανακουφιστική Φροντίδα δημιουργεί αίσθημα ασφάλειας στον ασθενή, καθώς γνωρίζει και νοιώθει ότι έχει συνοδοιπόρους στη νόσο ανθρώπους που, με πολλή αγάπη και εξειδικευμένη γνώση, θα τον στηρίξουν και θα τον βοηθήσουν να αντιμετωπίσει τις δυσκολίες, τις ανησυχίες και τους φόβους του.
Ανάλογα με τις ιδιαίτερες ανάγκες και επιθυμίες κάθε ασθενή που μπαίνει σε ένα πρόγραμμα Ανακουφιστικής Φροντίδας, η φροντίδα του μπορεί να γίνει σε μια ή περισσότερες από τις διαθέσιμες Υπηρεσίες.
Το όραμα όλων μας στη «ΓΑΛΙΛΑΙΑ» είναι να αποτελέσει και στην Ελλάδα η Ανακουφιστική Φροντίδα αναφαίρετο δικαίωμα για όλους τους ασθενείς που τη χρειάζονται.




Με κάθε σοκολατένιο αυγό που θα αγοράζετε από τα καταστήματά της, η Lapin House θα δωρίζει μέρος της αξίας του στους ασθενείς της «ΓΑΛΙΛΑΙΑΣ».
Έφτασε ή ώρα της Πασχαλινής Δωροαγοράς μας. Με μοναδικά δώρα για όλη την οικογένεια και τους αγαπημένους μας. Με όλους τους φίλους της «ΓΑΛΙΛΑΙΑΣ» που γίνονται μια αγκαλιά αγάπης για τους ασθενείς που δοκιμάζονται και τις οικογένειές τους. Σε περιμένουμε!
Η ΓΑΛΙΛΑΙΑ παρούσα όπως πάντα στα επιστημονικά δρώμενα, παρουσίασε την 14 χρονη εμπειρία της από την ενεργή προσφορά ανακουφιστικής φροντίδας, συμμετέχοντας σε Στρογγυλή Τράπεζα
Εγγραφείτε στο Newsletter μας